Preparing for a career in medicine
Medicine is an exciting and rewarding career. The training required to accomplish this goal will be extremely rigorous and take at least a decade, often longer, following completion of high school. Entry into medicine is highly competitive. You will need to demonstrate perseverance to complete the training, a strong desire to help others, a true intellectual curiosity about medicine in particular, and a love of learning in general. The following tips may assist to guide your decision.
- Complete Year 12 (high school or college) or your undergraduate degree.
- Complete any pre-requisite subjects. Before selecting your subjects for your senior school years, do your research to identify prerequisites and the courses to which they apply. Completing science pre-requisites during high school or your undergraduate degree is important, as it's much harder to complete these pre-requisites after graduation.Remember, choosing high-level mathematics, chemistry, physics, biology and English will stand you in good stead as you study medicine.
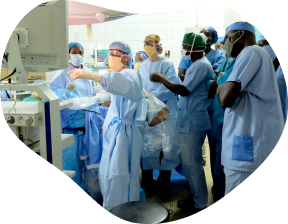
- Get involved. Take on leadership roles at your school and in your community to demonstrate you can motivate your peers to action, particularly in ways that benefit the school or community. Consider volunteering at a hospital, free clinic, doctor’s office or with a medical researcher. Volunteer work that is not directly medical related such as with a charity or other community service is also valuable.
Medical schools do not judge applications on work experience, but gaining some work experience demonstrates you have considered whether the demands of a caring profession is for you and that you are committed to studying medicine. - Take the UCAT or GAMSAT. Students interested in studying undergraduate medicine, dentistry and some other clinical science courses at a member university of the University Clinical Aptitude Test (UCAT) Consortium are likely to be required to sit the UCAT as part of their admissions process. Likewise, students wishing to study a postgraduate medicine degree are likely required to sit the Graduate Medical School Admissions Test (GAMSAT). Free guides for both the UCAT and GAMSAT are available. The GAMSAT test is offered twice a year, in March and September.
- Choose a university that fits your needs. To find the right medical school for you, consider academic reputation, size, distance from home, location, cost and of course their medical program. Apply to the medical schools that best suit your ambitions.
Scholarships. There is a range of scholarships available to study medicine at an Australian university. For Aboriginal and Torres Strait Islander students, the AMA Indigenous Medical Scholarship provides financial assistance for completing a medical degree, or search the Aurora Indigenous Scholarship Portal for further opportunities.
To learn more about preparing for a medical career, please visit Study Medicine. This site may assist you to identify and compare Australian university medical degrees - direct entry and degrees leading to undergraduate or postgraduate medicine.

Studying medicine
Studying medicine is challenging. Here are some practical tips to help you make the most of your time as a medical student.
- Have a balanced network. Medical students are famous for becoming very close knit and this is for good reason: as your work and routine become more stressful it is important to be able to talk to people in a similar position. However, it’s equally important to have non-medic friends too. One of the reasons you were accepted into medical school is because of your diverse range of interests and talents.
- Become an AMA Student Member. You will find the resources and advice to steer you through your medical career, and to provide assistance personally and collectively. All State AMAs engage with medical students either directly, through the MedSocs or via representative fora established by those organisations. The AMA has a student representative on its Federal Council – the peak policy-making body of the AMA.
- Join AMSA. The Australian Medical Students’ Association (AMSA) is the peak representative body for Australian medical students. AMSA is a vibrant student-run organisation that represents, informs and connects all of Australia’s medical students.
- Join your local Medical Society. Each medical school in Australia has its own medical student society, fondly known as a MedSoc. These are run by students who organise events, sports teams and nights out, which are a great way to get involved and meet people. They also provide plenty of helpful information and advice for getting through medical school and internship applications.
- Take it seriously. The behaviour and volume of work expected of you will be different from other students. You will need to juggle a lot of different elements simultaneously and this will take a level of maturity and time management. There are many ways to study. Don’t compare your methods with others. Find out what works for you.
- There’s more to medicine than reading textbooks. Learn what medicine is all about. Read the latest journal article, case report or reputable medical blog on topics that interest you. It will help bring together all the concepts you are studying and show you how to apply them in real life.
- Obtain copies of previous exams. The concepts will be similar, and reading and understanding these will give you a good idea of what to expect on your next exam.
- Keep an open mind. Throughout medical school you will meet a huge range of people and they can all teach you something. Seeing and doing as much as possible will enrich your time as a medical student. You may have your heart set on a speciality now, but most medical students change their mind as they progress.
- Enjoy yourself. Studying medicine is rigorous and overwhelming, so make sure you don’t burn out by setting aside time to regularly relax. Taking time to do things you enjoy will help you stay invigorated, enthusiastic and better able to cope with the pressures of medical school.
- Have a GP. If you are going to be a doctor, having your own GP to advise you on your health, fitness and wellbeing is invaluable.
On completing your medical degree, you receive provisional registration and enter the workforce as an intern or postgraduate year 1 (PGY1) doctor. This part of your training lasts for 12 months and is usually undertaken in a public hospital, although interns will increasingly spend part of their training in general practice, community-based settings and private hospitals. To successfully complete your intern year, you will be required to complete all mandatory core rotations (a medical, surgical & emergency medicine rotation) and normally two non-core rotations. You will also need to pass all your rotations in your intern year satisfactorily. Once you have completed your intern year you will receive general registration, which will be essential in progressing your career in all clinical and non-clinical medical pathways.
To learn more about becoming an intern, please log in as an AMA Member and visit ‘Pathways in Medicine’.
Planning your pathway
As the competition for medical training positions increases, proactively managing, planning and reviewing your career is a critical component of helping you secure that much-coveted role. Complete online leaning of interest available from the AMA’s doctorportal Learning, and the AMSA Academy to support your progression while studying medicine.
International Medical Graduates and Overseas Trained Doctors
International Medical Graduates (IMGs), someone with a medical qualification from a medical school outside of Australia or New Zealand, wishing to practise medicine in Australia, face a number of processes that must be completed in order to gain registration and employment.
Overseas Trained Doctors (OTDs) are medical practitioners who completed their core training overseas. An example of when an OTD may wish to apply to practice in Australia is as a result of workforce shortages, where the Australian Government encourages the immigration of doctors to a specific field.
Registration, Accreditation and Employment
There are several key factors relating to registration, accreditation and employment options that you have to consider when embarking on your medical career in Australia.
The Australian Health Practitioner Regulation Agency (AHPRA) and the Australian Medical Council (AMC) are your first contact points when seeking employment in Australia as medical officers. They provide the information and pathways relevant to obtaining certification of your medical degree and your medical registration, which is a requirement for practising medicine in Australia.
‘Doctor Connect’, an Australian Government Department of Health initiative helps IMGs understand the steps required to work as a doctor in Australia, where they can work and restrictions on billing patients under Medicare.
Student membership
AMA Student Members
The Australian Medical Association (AMA) is the most influential membership organisation representing registered medical practitioners and medical students of Australia. As Australia’s future workforce, the AMA supports medical students studying in Australia.
Advocacy
The AMA represents you on the important issues that affect you now while at university, and during your future career in medicine. We lobby on behalf of our student members on funding for medical school places, intern and specialty training positions, and ensure the adequate provision of work and training places for graduating students.
Networking
The AMA provides you with opportunities to meet and socialise with other medical students, attend training forums, access mentoring programs, and gain advice from leaders and influencers.
Benefits and Resources
Becoming an AMA Student Member is FREE. You will have access to a range of member-only benefits and resources at the national and state or territory level. This includes online learning that may support your studies.
AMSA Members
The Australian Medical Students Association (AMSA) is the prime membership organisation for medical students in Australia.
As a medical student studying in an Australian university, membership of AMSA is automatic, giving access to a range of member benefits, events, and educational, social and leadership opportunities. You can get involved with AMSA through your university Medical Society and interest groups or nationally via AMSA networks and events.
To join AMSA, click here.
Working Together
Together, the AMA and AMSA recognise that medical students are the future of medicine in Australia. The AMA supports and works with AMSA in representing the interests of medical students in Australia and is your collective voice on national issues. AMSA and the AMA encourage medical students to join both organisations.
Disclaimer
This material is generic in nature and is made available on the understanding that the AMA is not engaged in rendering professional advice. Before relying on the material provided, users should carefully evaluate its accuracy, currency, completeness and relevance for their purposes, and should obtain professional advice relevant to their particular circumstances where necessary. Whilst every effort has been made to ensure the accuracy of the information provided, the AMA or its employees cannot be held responsible for any loss or damage arising to any person as a result of using this site.