Stakes high as antimicrobial resistance accelerates globally
The AMA has called for three solutions to antimicrobial resistance in a new report.
The AMA has called for three solutions to antimicrobial resistance in a new report.
In its new report, Antimicrobial resistance: the silent pandemic, released to coincide with World Antimicrobial Awareness week, the AMA has called for:
- establishing a Centre for Disease Control (CDC) that is a recognised separate authority for the national scientific leadership and coordination of diseases and health threats, as well as several immediate priorities for government to ensure Australia’s response to antimicrobial resistance is effective, integrated, and aligned to One Health objectives
- improving antimicrobial stewardship practices in Australia, by embedding stewardship practices, education and training, and clinical decision support tools into all sectors
- improving the antimicrobial market through sovereign manufacturing of antimicrobials and implementing mechanisms to incentivise research and development.
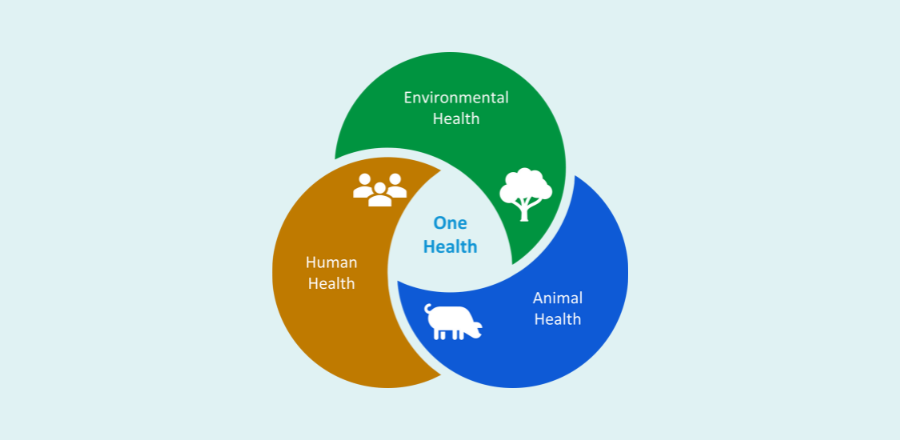
While Australia already has a National Centre for Antimicrobial Stewardship the AMA says a CDC would have a broader remit and would encourage a One Health system view and make it easier to apply antimicrobial resistance strategies across all policy areas.
A One Health system takes a wholistic approach to health seeing the interconnectedness of human and animal health and the environment.
The AMA report says while antimicrobial resistance is a natural phenomenon, the largely unrestrained use of antimicrobials in human and animal health and agriculture combined with several other complex factors, including climate change and globalisation, is accelerating the emergence and spread of resistant pathogens.
Of these factors, the failing market for antimicrobial development has meant that the breadth and novelty of the current pipeline of new antimicrobials is insufficient to meet the ongoing threat of antimicrobial resistance.
Highlighting the issue in the media AMA President Professor Stephen Robson said without new antimicrobials, the world may be on track to return to the medical “dark ages”, a time where a superficial scratch could be life threatening, and the procedures and treatments which we now rely on are considered too risky to perform, due to risk of untreatable infection.
He said antimicrobial resistance is one of the most serious global health threats of the 21st century which will undermine healthcare systems and food safety and supply, and result in millions of deaths.
The AMA report says if the problem is not addressed antimicrobial resistance will be a leading cause of death by 2050.
“The best evidence we have is that by 2050 the annual impact of antimicrobial resistance on the Australian economy will be $142–283 billion, and $80–90 trillion globally. This is not something we can wait to address ― the stakes for all of us are far too high,” Professor Robson said.



